
Decision-support needs of people with co-occurring depression and problematic alcohol use
Researchers at the Matilda Centre conducted a needs assessment to help us better understand and address the unmet needs of people with problematic alcohol use and comorbid depression when making decisions about early intervention and treatments.
Depression and problematic alcohol use is common, highly burdensome, and frequently co-occur, affecting around 2.5 million Australian adults. Despite a number of effective treatment options available, healthcare workers aren't provided with guidelines to support decision making for individuals with co-occurring disorders. This results in tens of thousands of individuals having unmet treatment needs.
To meet this need, researchers at the Matilda Centre conducted a needs assessment to guide the development of patient decision-support resources to promote shared decisions, and the informed, timely update of guideline-consistent treatments.
Our approach
This world-first initiative incorporated views from patients, clinicians and families, resulting in a comprehensive, decisional needs assessment for people with co-occurring depression and problematic alcohol use. This survey forms part of an initial program of research to develop and evaluate evidence-based, co-designed resources to improve shared treatment decision-making and outcomes for people with common mental health and alcohol/other drug use issues, namely depression and problematic alcohol use.
The survey was conducted online in mid 2019. The research team recruited a total of 56 patient-consumers, 65 clinicians, and 16 family members (aged 18+) with experience of making decisions about treatment for their own, or a patient’s, problematic alcohol use and co-occurring depression. Participants were recruited via social media, e-newsletters, and websites of leading Australian-based professional societies, as well as consumer-and carer-based mental health and substance use organisations.
Key findings
Key findings from the needs assessment include:
- Patients face a range of difficult decisions in the initial stages of treatment seeking. These include decisions about:
- starting medications,
- counselling or psychotherapy, and
- whether to prioritise treating their depression or alcohol use.
- When facing these decisions, patients reported feeling uninformed and unsupported. A lack of clarity about the importance of different treatment options led to an inability to make an informed, effective decision that they would feel confident in implementing (i.e., high decisional conflict). Clinicians reported even higher decisional conflict than patient-consumers themselves.
- Most participants reported preferences for shared treatment decisions between patients and clinicians. However, patients were more likely than clinicians to report that they felt that treatment decision-making was clinician-led.
- Perceptions of involvement in treatment decision-making differed between patient-consumers and clinicians. A greater proportion of clinicians felt that patient-consumers were as involved as they wanted to be in making treatment decisions; however, about a third of patient-consumers reported not being as involved as they would like.
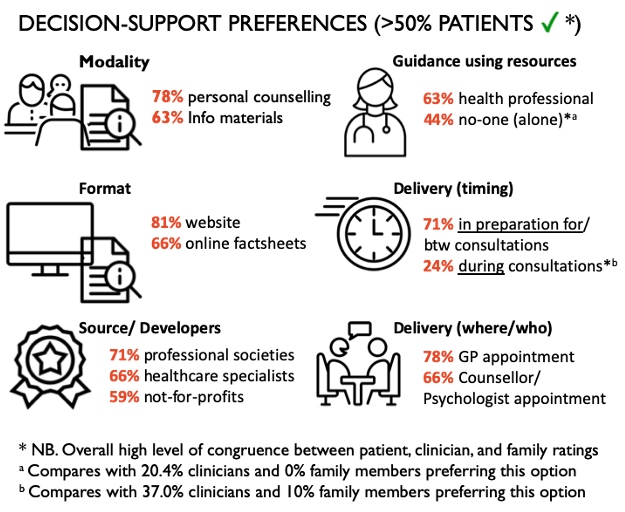
- As seen in the below, patients’ decision-support preferences included online information from reputable organisations delivered in advance of, or between, consultations with a GP and/or counsellor/psychologist. Most patients would like a health professional to guide them through using these resources, but a large proportion would also prefer to use these independently.
What's next
With a better understanding of stakeholder needs, the research team are now using findings to guide the content, format and delivery of new resources to support informed decision-making about early intervention and treatment for people with problematic alcohol use and depression.
This research was led by Postdoctoral Research Fellow, Dr Alana Fisher, whose background is in the development and evaluation of evidence-based decision-support tools to aid shared treatment decision-making for people with mental health conditions.
Other members of the research team include: NHMRC Senior Research Fellow and Director of Early Intervention and Treatment Research at the Matilda Centre Professor Katherine Mills, NHMRC Translating Research Into Practice (TRIP) Fellow, Dr Christina Marel and the Matilda Centre Director Professor Maree Teesson.
For more information on this project, please contact Dr Alana Fisher at a.fisher@sydney.edu.au.