
Heart disease & stroke research receives $12.4 million federal funding boost
The Minister for Health, the Hon Greg Hunt MP announced today $29 million to address one of the leading causes of death in Australia – including $12.4 million in funding for University of Sydney-led research initiatives that will reduce the health burden for people affected by stroke and heart disease.
Funding will be directed into four key projects at the University: investigating the potential of an anti-inflammatory drug for patients affected by stroke; the design of a more durable biocompatible heart valve; investigating how to help people lead active lives with congenital heart disease – the most common of all inborn abnormalities in Australia; and the establishment one of the most extensive datasets profiling congenital heart disease in Australia.
This funding is the first round of disbursements from the Government’s 10-year, $220 million investment to boost research into heart disease and stroke through the Medical Research Future Fund’s (MRFF) Cardiovascular Health Mission.
Each year, one in five Australians are affected by heart disease and stroke, one Australian dies of cardiovascular disease every 12 minutes, and one Australian experiences a heart attack or stroke every five minutes.
Professor Robyn Ward, Pro Vice-Chancellor and Executive Dean of the Faculty of Medicine and Health, said:
“This is an outstanding outcome for our researchers dedicated to identifying and solving some of the biggest issues in cardiovascular disease.”
“Their work is testament to the innovative and wide-reaching research conducted at the University of Sydney, that draws upon the collaborative expertise and strengths of academics from different disciplines.”
Professor Anthony Keech will be leading a project to study an anti-inflammatory tablet that could potentially benefit high-risk patients who have survived a stroke.
A safer alternative for post-stroke patients
Professor Anthony Keech, Deputy Director of the NHMRC Clinical Trials Centre and cardiologist from the Royal Prince Alfred Hospital from the University of Sydney School of Medicine will be leading a project awarded $3 million to investigate an anti-inflammatory tablet to potentially benefit high-risk patients who have survived a stroke.
Inflammation plays a critical role in the rupture of artery plaques, leading to acute stroke. Despite current best treatments, many people remain at high risk of recurrent stroke events, predominantly because current therapies do not specifically target the inflammatory component of arterial disease.
The Colchicine After Stroke to Prevent Event Recurrence (CASPER) project will investigate the ability of colchicine, a safe and commonly used anti-inflammatory drug, to inhibit vascular disease-associated inflammation and improve clinical outcomes.
Professor Keech is also lead investigator in the Immune-Modulating Particles and Colchicine To Improve COVID-19 Outcomes (IMPACT-ICO) project, also included in an announcement this month, which was recently awarded $980,415 from the Medical Research Future Fund.
IMPACT-ICO will also investigate colchicine and its anti-inflammatory properties in the context of reducing the inflammatory response to a viral infection such as the pathogen causing COVID-19. In a clinical trial, the project will test Colchicine and a novel, biodegradable particle which reduces inflamed cells in the hope that this can improve medical outcomes for patients infected by the virus.
Improving quality of life for people with congenital disease
Each year in Australia, it is estimated 2,400 babies are affected with congenital heart disease. People with complex and severe congenital heart disease require specialist treatment throughout their life.
Dr Rachael Cordina, clinical senior lecturer at the Sydney Medical School, will lead the Congenital Heart Fitness Intervention Trial (CH-FIT) conducted at the University and will receive $3.3 million grant support. CH-FIT will investigate the health impact of exercise, and the best way to help adults and children living with congenital heart disease to lead active lives.
Most Australians who have congenital heart disease survive to adulthood but often live with complex medical problems. Although regular exercise is well-recognised as beneficial for physical and mental health in many health conditions, there is a lack of research investigating the optimal way to encourage active lifestyles for people with congenital heart disease.
This project will address that gap with a 12-month exercise training and lifestyle education program designed to improve exercise capacity in children and adults.
It is the largest and most definitive exercise trial ever performed in people living with congenital heart disease.
A more durable heart tube and valve design
Professor David Winlaw, the Vivienne and Ross Hobson Professor in Paediatric Cardiac Disease in the Faculty of Medicine and Health and paediatric cardiac surgeon at The Children’s Hospital at Westmead is part of a team leading efforts to develop a biocompatible tube with a synthetic heart valve to be used in reconstructive surgery for congenital heart disease, which has been awarded $2 million in funding.
A multidisciplinary team of doctors, scientists and engineers will bring together the most recent developments in polymer science and computational engineering. The goal is to build a durable and biocompatible right ventricle to pulmonary artery valved tube used in reconstructive surgery for congenital heart disease.
Currently available animal and donated human products fail in just a few years, requiring replacement open heart surgery every 5-10 years.
The project will design a product tailored to the individual that will allow the tube to ‘grow’ with the child, maintain good valve function, avoiding repeated surgeries, improving heart function and quality of life.
Mapping the impact of congenital heart disease in Australia
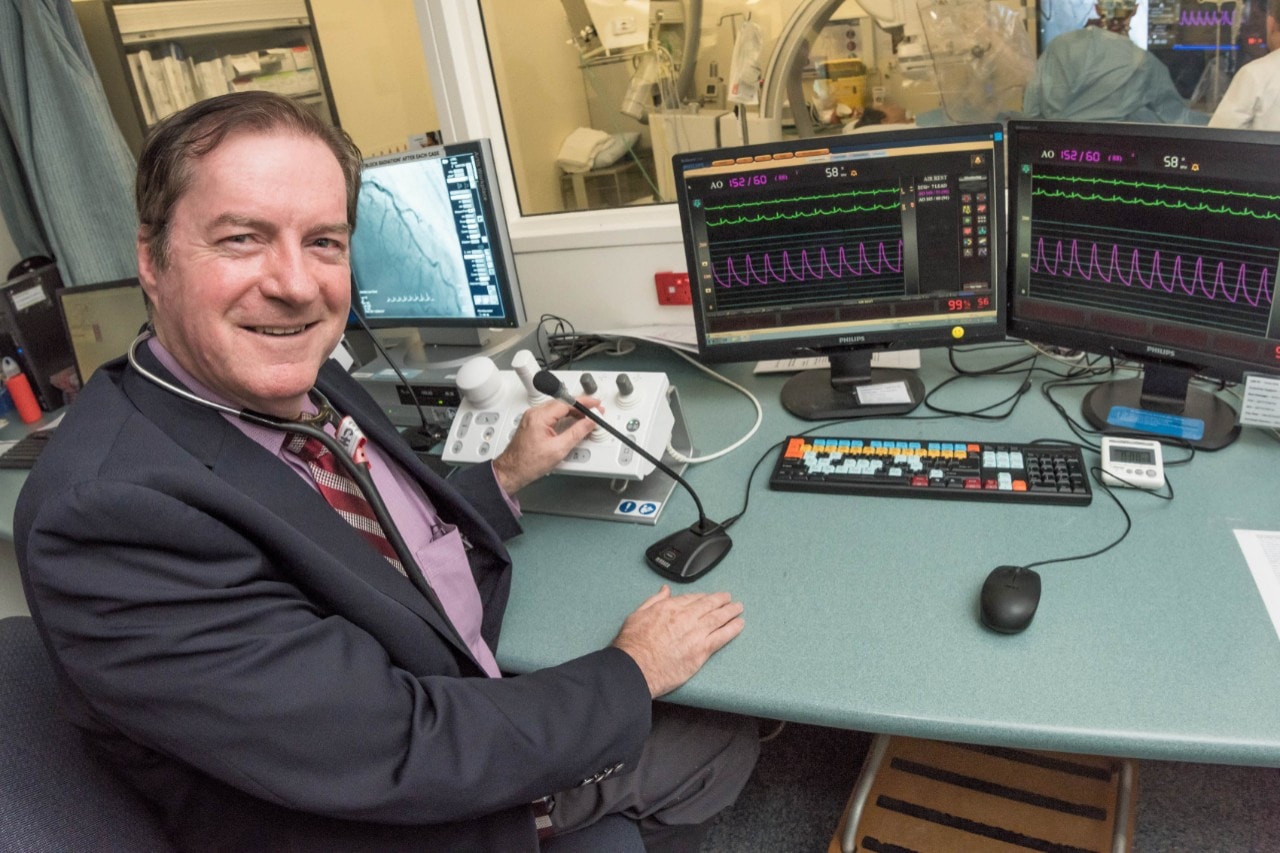
Professor David Celermajer, Scandrett Professor of Cardiology at the Sydney Medical School and head of the discipline of cardiology in the Faculty of Medicine and Health, will lead a study awarded $4 million in funding to produce one of the most extensive data sets profiling the burden of congenital heart disease in Australia.
Professor Celermajer is also director of Adult Congenital Heart Services at Royal Prince Alfred Hospital and clinical director of the Heart Research Institute.
The national multi-disciplinary project will establish and analyse demographic and clinical data describing the outcomes, experiences and burden of congenital heart disease for a cohort of Australians who were born with the condition.
The information will help influence management, care and support to target critical psychological, mental health, neurocognitive and quality-of-life outcomes in congenital heart disease patients and the parents of children with congenital heart disease.
Congenital heart disease affects more than 100,000 Australians. The project, to be led from the Royal Prince Alfred Hospital, will be carried out at over 10 sites across all six states in Australia.