Publication list
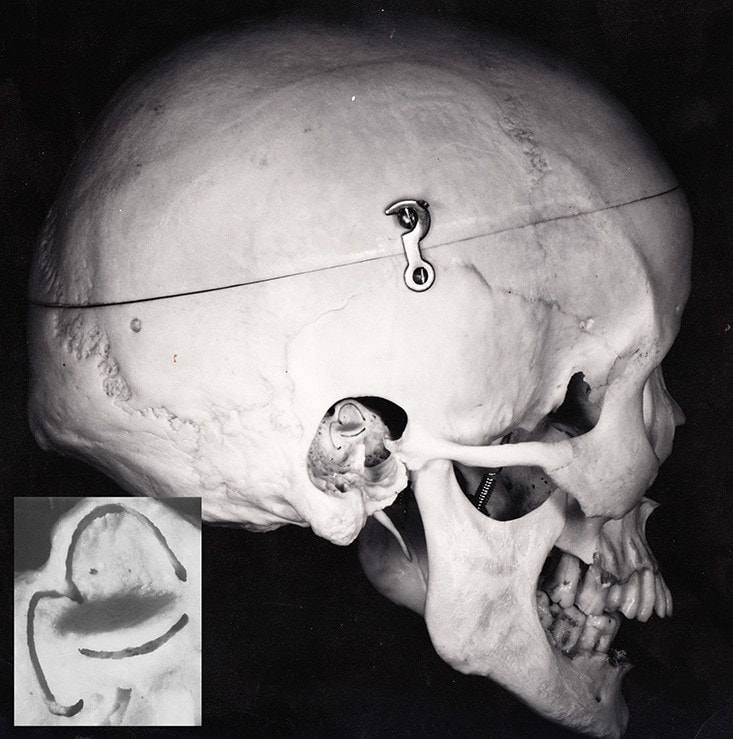
View of the skull from the right-hand side: the temporal bone has been dissected, showing the orientation of the semicircular canals in the head.
Our laboratory works closely with researchers at the Hearing and Balance Clinic at Royal Prince Alfred Hospital; this collaboration facilitates the rapid translation of research findings into new tests and treatments for patients suffering from balance disorders.
This 1m centrifuge for human subjects radius allows to be accelerated to angular velocities of up to 300 degrees per second, providing simultaneous linear and angular stimuli to the vestibular system, allowing tests of both otolith and semicircular canal function.
Recent modifications to the centrifuge allow subjects to be rotated while lying supine, or on their side. This will enable us to explore whether the saccular macula, one of the otolith organs, has a role in controlling eye movements.
This chair allows whole-body static tilts for human subjects, during which ocular counterroll and/or perception of tilt can be measured, for tests of otolith function. Another tilt chair allows us to deliver static pitch tilts, and is presently being used in studies of vergence eye movements.
Our 6m sled allows sudden linear accelerations to be delivered safely to human subjects or guinea pigs, while their eye movements, perceptual, or postural responses are measured. A recent study with this sled showed unexpected head movements in some normal human subjects in response to brief linear accelerations – these results may be significant in understanding whiplash injuries in car accidents.
The Optotrak system (Northern Digital, Waterloo, Ontario, Canada) measures rotations and translations with 6 degrees of freedom for the high-speed, accurate study of head and body movements. The system works by tracking small infrared light-emitting diodes (LEDs) with three line-scan cameras. We use Optotrak to measure postural changes in human subjects and guinea pigs during acceleration on the linear sled.
This small turntable for testing guinea pigs can be rotated in the animal’s yaw plane. The turntable is mounted on a swing, allowing tilts to be delivered in either roll or pitch, depending on the initial orientation of the animal on the turntable. Static and dynamic pitch or roll stimuli can thus be delivered to guinea pigs while eye movements are measured, or during single-unit recording to identify the function of the neuron being recorded.
Vestibular stimulation produces characteristic eye movements or Vestibular Ocular Reflexes (VORs). The spatial components of VORs have been attributed to activation of specific vestibular sensory regions: stimulation of a semicircular canal (SCC) mainly produces nystagmus around an axis roughly perpendicular to the plane of that canal, whereas stimulation of the otoliths mainly produces changes in ocular torsional position.
Galvanic vestibular stimulation (GVS) of human subjects by currents as large as 5mA can be delivered safely and painlessly through large-surface-area electrodes on the mastoids, producing a range of vestibular responses including characteristic eye movements. With video measures of 3d human eye movements during prolonged GVS, we have been able to observe that normal subjects show eye-movement response patterns which could be expected from stimulation of a combination of vestibular sensory regions, and to make a model of patient responses which is consistent with the particular vestibular disorder.
The VidEyeO Eye-movement recording system, an updated version of the VTM (Video Torsion Measurement) system provides accurate measures of three-dimensional eye position. Eye movements are recorded with small infrared cameras which are usually mounted on a Sansplint mask individually moulded to the subject’s face, thus preventing spurious movement of the cameras with respect to the eyes. Images of the eyes are recorded to video tape or processed online during the test. During data processing, horizontal and vertical eye positions are measured from the centroid of the pupil in the video image. Ocular torsion is measured by doing a cross-correlation of the pattern of iral striations.
We are continuing to develop this recording system for use in the clinic. A new lightweight, light-occluding headset and mobile acquisition system using digital (Firewire) cameras and a laptop computer now provides the opportunity to do testing at the bedside. Modified versions of the eye-movement-analysis software have been used by other research groups at the University of Sydney. Dr Diana Caine of the Visual Perception Unit has recently used a version of the system to compare the scan paths, during face-recognition tasks, of normal subjects with those of prosopagnosic patients.
The current system for measuring ocular torsion requires the use of Pilocarpine eye drops to constrict the pupil. We are now investigating the use of scleral markers so we can obtain accurate ocular torsion without the need for pupil constriction. We have recently implemented this method successfully in guinea pigs.
